"Taking part in research gave me control and dignity in the face of cancer treatment"
- 20 May 2022
- 3 min read
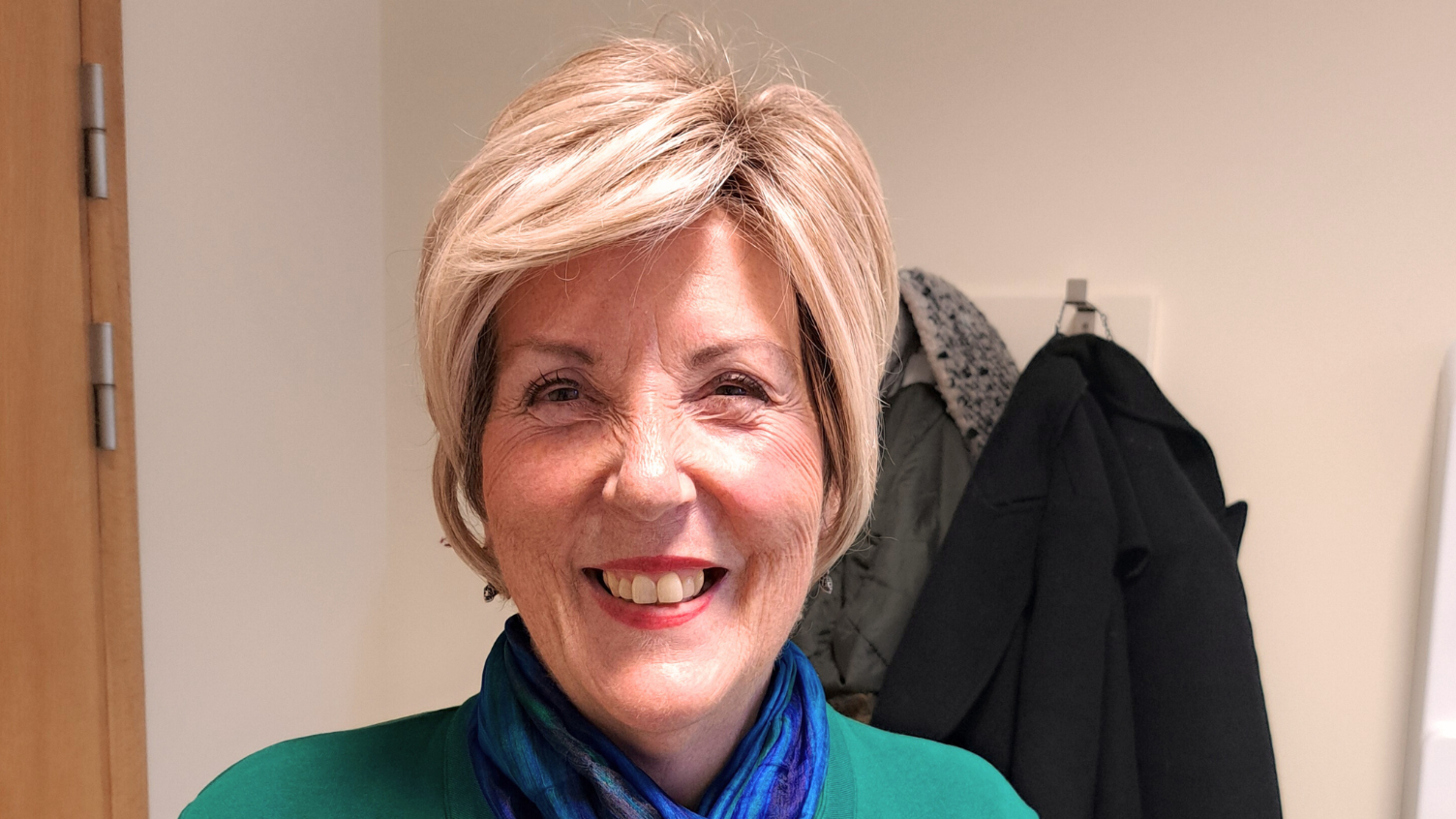
A passionate advocate for research in the palliative care setting, Jan jumped at the chance to volunteer for a study when she realised she was eligible. This is her story.
As a former nurse and midwife, Jan from Somerset knows more than most the benefits of taking part in research.
First diagnosed with breast cancer in 2008, Jan continued working until November 2021, finally retiring on grounds of ill health five years after her cancer was found to have returned. Jan receives care at home from the community team at St Margaret's Hospice, where she previously worked.
"I'm Jan, I'm 63 and I live in Taunton, and I was diagnosed with breast cancer in 2008, when I was 49. A routine mammogram found three tumours, and I was treated with surgery and chemotherapy. In 2016 the cancer returned, and it's now in my pelvis and my spine. I feel very fortunate the original mammogram was done when it was done, because if it had been left any longer I don't think I would be here now. I'm very grateful and I consider myself lucky.
"I trained as a nurse in 1982, and research wasn't on the agenda then. You just did your job and learned about new things kind of by word-of-mouth. I held various jobs, and one year I went to the national end of life conference in Liverpool, because I had two posters on display relating to the work I had done at the hospice, and attended all the lectures. I came away with a strong sense of the importance of research in end of life care in particular.
"Going back to work, I heard of the StOIC (Study of Opioid-Induced Constipation) research. I was handing out the pills on the inpatient unit, so I knew the medications that the patients were having, and the problems they were experiencing. As part of my pain control, I was taking some morphine, which is an opioid. So it dawned on me that actually, I could be eligible.
"I found taking part in the research and taking the medication very straightforward. I didn't need to take it every day, which was good because I was already on loads of medication. I found a balance, between needing the morphine twice a day, every day to control the pain, and being able to use the medication when I needed it. The pattern that I evolved worked really well, and the medication was far more effective than the alternative.
"It allowed me to be mobile, which I needed to be as I was working, and made a huge difference to me and the options that I had. Really, the constipation just felt like another thing to mess up your life. You're on all this medication, you're taking morphine with the side effects of that, and on top of everything the constipation made you feel sick and bloated.
"I felt more in control as well, so there was no question that I would get stuck, which is really important for your self-esteem. When you have cancer, things become more public than they would normally be. The medication means you have a bit more control over something private and you just have a bit more dignity.
"That's a real positive for this particular medication, and I only came across it through taking part in research. I would imagine there are a lot of people on opioids, and a lot of people suffering from the side effects, and those problems could be resolved in time.
"I feel passionately about research in palliative care. The end of life comes to us all, and as patients and as healthcare professionals, we only get one chance to get it right. By sharing experiences and basing our practice on research, we can all learn, and make the patient experience better."
Find out how you could become a Trialblazer by volunteering for research: https://bepartofresearch.nihr.ac.uk/trialblazers/